Heat Illness
Heat illnesses are serious medical conditions. If not properly identified and treated, serious organ damage can occur, which may be fatal. Heat illnesses can be avoided if the proper steps are taken. As Tactical Athletes, you need to be aware of your surroundings and limit your risk factors. All Tactical Athletes’ work as part of a team, it is important to look out for each other.
By: J. Scott, DPT, ATC
New England weather varies greatly between the four
different seasons. The frigidly cold
temperatures of winter with snow and ice are a stark contrast to the hot and
humid summer months. Currently in the
middle of summer, New England has been battling scorching high temperatures
during the month of July.
As Tactical Athletes are required to work in any and every
weather condition, they are both particularly susceptible to sustaining heat
illnesses themselves, if not treating the general public suffering from these
conditions. There are four general
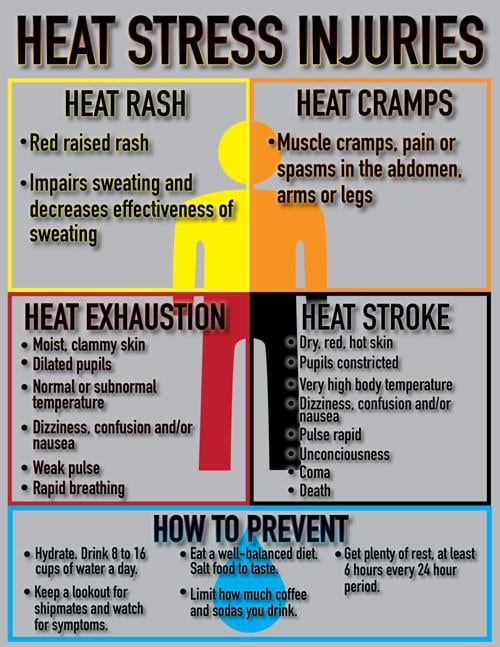
classifications of heat illness:
· Heat cramps:
Muscle cramping caused by exercising and/or working in high
temperatures, with inadequate replacement of fluids and/or electrolytes.
o
Signs/symptoms:
Muscle pain, spasm, contraction.
o
Treatment:
Stop activity, rehydrate, electrolyte replacement, gentle stretching of
the affected muscles. If prolonged heat
cramping occurs, seek medical treatment.
· Hyponatremia:
Decreased levels of blood sodium levels.
During vigorous activities, Athletes sweat. Sweat consists of water and
electrolytes. Both water and
electrolytes need to be replaced by the Athlete. If fluid levels are replaced, but
electrolytes (sodium is an electrolyte) are not also replaced an imbalance of
blood sodium levels occur.
o
Signs/symptoms:
Headache, mental confusion, nausea, vomiting, extremity edema, excessive
water consumption.
o
Treatment:
Electrolyte replacement. For
severe symptoms consult a physician.
· Heat exhaustion:
Classified as a moderate illness caused by completing strenuous physical
activity in hot and humid environments.
This condition is characterized by decreased cardiac output.
o
Signs/symptoms:
Dizziness, diarrhea, depleted energy, decreased coordination, fainting,
headache, nausea, vomiting, profuse sweating, pale skin, stomach cramps, core
temperature <104°F/40°C, central nervous
system dysfunction.
o
Treatment
§
Immediately remove from activity
§
Seek a cool and shaded environment
§
Remove excess clothing and equipment
§
Lay down with legs elevated above the heart
§
Rehydrate with oral fluids and/or IV normal
saline
§
Place ice packs behind the back of the neck,
under the arms, in the groin, and behind the knees
§
Monitor vital signs
§
Transport to an emergency medical facility
o
Return to activity: Follow-up with a physician, consult a
Certified Athletic Trainer on proper return to activity guidelines.
· Exertional heat stroke: Identified as the most severe heat
illness. This condition is an elevated
core body temperature ≥104°F/40°C, caused by strenuous
physical activity in increased environmental temperatures. When the core body temperature reaches these
high levels, there is central nervous system abnormalities and organ system
failure. If not identified and treated
quickly, this condition is life threatening and potentially fatal.
o
Signs/symptoms:
Altered consciousness, confusion, combativeness, decreased blood
pressure, decreased mental acuity, diarrhea, dizziness, headache, increased
breathing rate, irrational behavior, nausea, vomiting, hot and wet or dry skin
(individual may have stopped sweating), weakness, seizures, core temperature ≥104°F/40°C, central nervous
system dysfunction, organ failure.
o
Treatment
§
Immediately remove from activity
§
Remove excess clothing and equipment
§
Whole body cooling performed as quickly as
possible. This is best achieved through
cold water immersion. If cold water
immersion is not possible, place the individual under cold, running water or
place ice packs behind the back of the neck, under the arms, in the groin, and
behind the knees. The individual’s core
body temperature must be cooled as quickly as possible to limit organ
damage.
§
Monitor vital signs
§
Start an IV of normal saline
§
Once the core body temperature has decreased to
101°F - 102°F, the individual should
be immediately transported to an emergency medical facility.
o
Return to activity: Follow-up with a physician, physician
clearance to return to physical activity, consult a Certified Athletic Trainer
on proper return to activity guidelines.
Ways to prevent heat illness:
·
Stay well hydrated before, during, and after
strenuous activity
·
Take multiple rest breaks during strenuous
activity if possible
·
Acclimatize to the heat
·
Practice good nutrition
·
Get enough sleep
·
Regularly exercise
·
Limit excessive caffeine, drug, and alcohol
intake in warmer weather
·
Stop physical activity if signs or symptoms of
heat illness occur
·
Look out for your fellow Tactical Athletes
Heat illnesses are serious medical conditions. If not properly identified and treated, serious organ damage can occur, which may be fatal. Heat illnesses can be avoided if the proper steps are taken. As Tactical Athletes, you need to be aware of your surroundings and limit your risk factors. All Tactical Athletes’ work as part of a team, it is important to look out for each other.
By: J. Scott, DPT, ATC
Sources:
The National Athletic Trainers’ Association position statement
on Heat Illness
The Centers for Disease Control Heat-related illness

Comments
Post a Comment